

রোগতত্ত্ব, রোগ নিয়ন্ত্রণ ও গবেষণা ইনস্টিটিউট
গণপ্রজাতন্ত্রী বাংলাদেশ সরকার
আপনার মতামত প্রদান করুন
কনটেন্টটি শেষ হাল-নাগাদ করা হয়েছে: বুধবার, ১৮ জুন, ২০২৫ এ ০৬:৩০ PM
Surveillance Report, 2024
কন্টেন্ট: পাতা
An update on the disease surveillances carried out at IEDCR in 2024 is presented here. Individual details are available in the “surveillance” tab of iedcr.gov.bd. Links are also provided at the end of each updated surveillance. Readers may also check Volume-4 Issue-2 of NBPH which provides a detailed information on the history of the various disease surveillances carried out in Bangladesh at:
NBPH; Volume-4; Issue-2: /pages/static-pages/6922dc05933eb65569e0dff6
Anthrax Surveillance:
Anthrax surveillance is continuing in three upazila of Meherpur district.
• In 2024, from January to August, 65 samples were received from sentinel sites, of which 34 were positive for Bacillus Anthracis. All cases were from Gangni and Sadar Upazila of the Meherpur district.
Anthrax Surveillance: /pages/static-pages/6922de53933eb65569e19deb
Leptospirosis Surveillance:
Since 2019, IEDCR has been conducting leptospirosis surveillance in 8 sentinel sites throughout the country.
Table 1: List of leptospirosis surveillance sites with positive cases (Jan to Jul ’24)
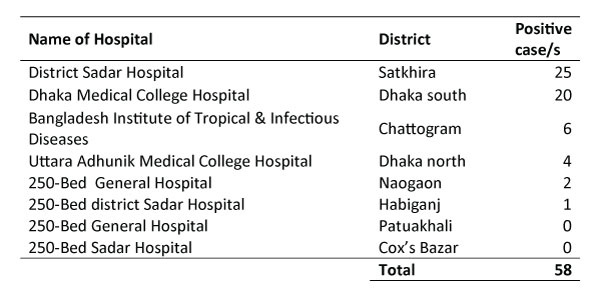
Most of the positive cases were identified from the districts of Satkhira and Dhaka (Table 1).
Hospital Based Rotavirus and Intussusception Surveillance (HBRIS):
In Bangladesh, the estimated incidence of rotavirus in the under-fives is 10,000 cases per 100,000 children. IEDCR and icddr,b jointly started HBRIS surveillance since 2012.
Table 2: Sample collection and rota virus positivity in 2024
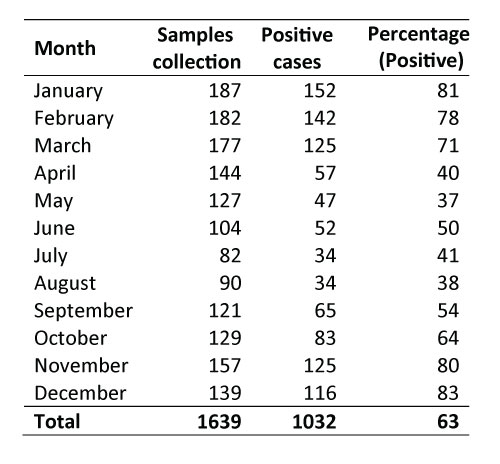
The proportion of rotavirus positivity is higher from January to March. Then again, an upsurge is seen in November and December (Table 2).
From 2012 to Jun 2024 the proportion of rotavirus positivity showed a seasonal variation with an upsurge between November and February with a peak in January. In the last 3 years, the positivity was found to have increased in the month of March also.
Hospital Based Rotavirus and Intussusception Surveillance (HBRIS):
/pages/static-pages/6922de0a933eb65569e17bed
National Influenza Surveillance:
Since 2017, the National Influenza Centres (NICs) has been conducting two surveillance programs, NISB (National Influenza Surveillance Bangladesh) and HBIS (Hospital Based Influenza Surveillance). NISB is coordinated by IEDCR since 2010 in 10 sentinel sites. HBIS is coordinated by IEDCR and icddr,b since 2007 in 9 sentinel sites across Bangladesh.
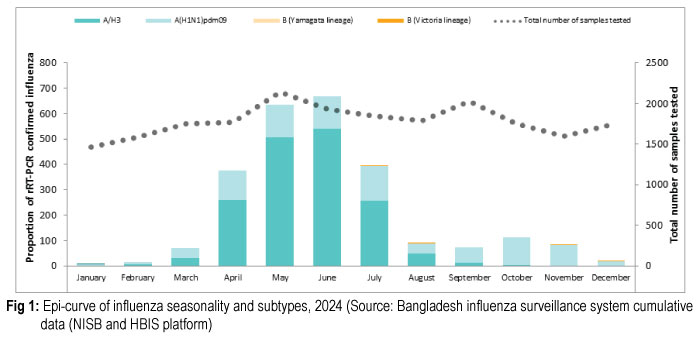
During 2024 A(H1N1)pdm09 and A/H3 subtypes were detected. The proportion of positive influenza cases were high from April to July which coincides with our regular seasonality which is March to September.
NISB Monthly Reports: /pages/static-pages/6922dd88933eb65569e155ff
HBIS Monthly Reports: /pages/static-pages/6922e142933eb65569e2b2d3
Nipah Surveillance:
IEDCR is conducting the Nipah virus (NiV) surveillance since 2006. Currently, it is running in 14Government facilities. including 12 government medical college hospitals and 2 district hospitals covering 8 divisions of the country. The objectives of the surveillance are to detect outbreaks of NiV infection, modes of transmission and identify possible risk factors.
Table 3: Distribution of Nipah cases in Bangladesh (session 2023-24)
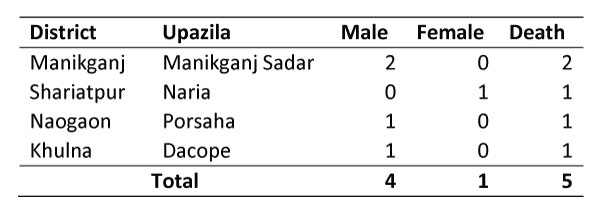
In the 2023-24 session, five cases of NiV infection were detected in 4 districts of Bangladesh. Among them, 4 were males and 1 was a female. All of them had history of raw Date Palm Sap (DPS) consumption. The fatality rate was 100% (Table 3).
Nipah Virus Transmission in Bangladesh: /pages/static-pages/6922dd6c933eb65569e14fc2
AMR Surveillance:
The Antimicrobial resistance (AMR) surveillance system in Bangladesh is unique as it currently integrates both case-based and lab-based approaches, as recommended by the Global Antimicrobial Resistance and Use Surveillance System (GLASS). The case-based surveillance started from 2017 and the lab-based surveillance was initiated in 2022. Case-based surveillance is conducted in 11 sites nationwide, while lab-based surveillance is conducted in 21 public and private laboratories.
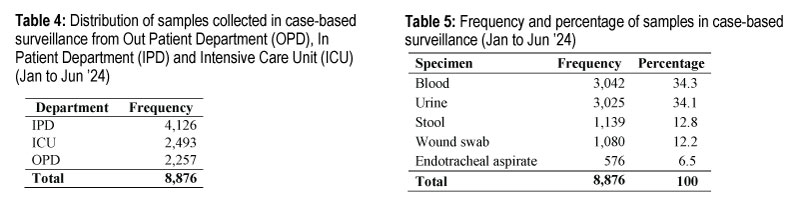
Most number of samples were collected from the IPD (Table 4) of which blood and urine samples comprised the most (Table 5).
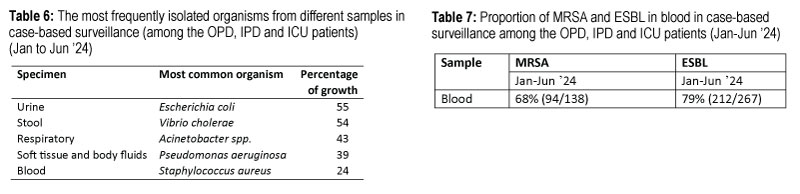
The most isolated organisms in different samples were E. Coli in urine, V. Cholerae in stool, Acinetobacter spp. in respiratory, Pseudomonas aeruginosa in soft tissue and body fluids, Staph. aureus in blood (Table 6). The status of MRSA (Methicillin-resistant Staphylococcus aureus) and ESBL (Extended-spectrum beta-lactamase) reflects the situation of AMR. The percentage of MRSA and ESBL were 68 and 79 respectively. This could be explained by the high percentage of patients coming from the ICU (Table 7).
To see the antibiogram and detailed information (including live AMR Onehalth dashboard), please visit the link below:
/pages/static-pages/6922dcde933eb65569e1277d
Child Health and Mortality Prevention Surveillance (CHAMPS):
The primary objective of CHAMPS is to identify the precise causes of stillbirths and deaths among children under five years of age. IEDCR has been conducting the CHAMPS activities from 2017 in collaboration with the icddr,b. The facility-based surveillance is conducted in 1 upazila of Rajbari district and 6 upazilas of Faridpur district. Community mortality surveillance was established in 2019 in Baliakandi, Rajbari.
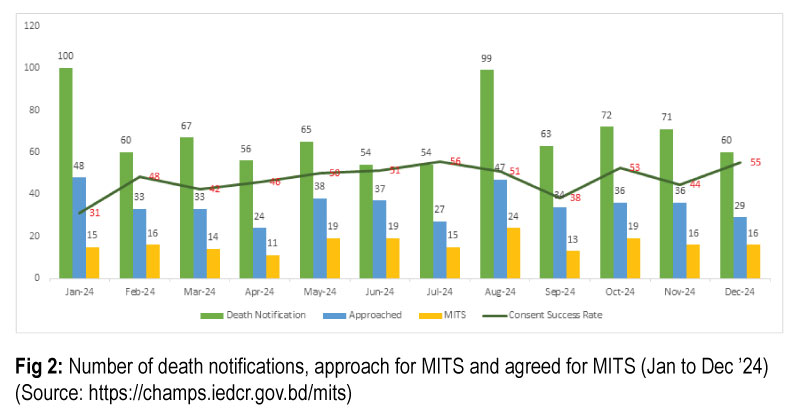
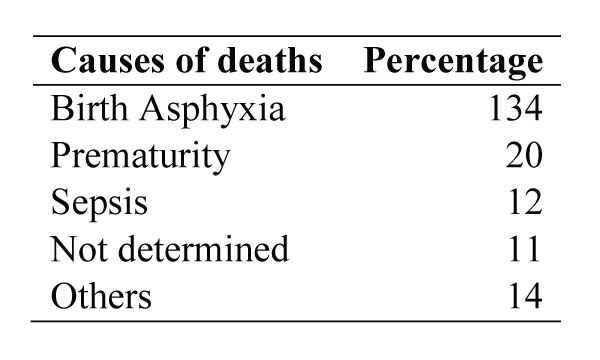
Table 8: Causes of deaths of children, Jan-Dec 2024 (N=191)
The number of death notifications and approaches for MITS reached their peak in January and August 2024 (Fig 2). The consent success rate has also increased over the year. This increase can be attributed to robust community engagement activities and effective coordination with government and private stakeholders. Between January and December 2024, CHAMP BD team conducted 197 MITS, comprising 110 stillbirths, 64 early neonatal deaths, and the remainder being infants. Of these, 55 cases originated from Baliakandi, Rajbari, while the others were from the six upazilas of Faridpur known as expansion area.
During this period, a total of 191 deaths were investigated. The majority causes of deaths were birth asphyxia (70%, 134/191), prematurity and related complications (10%, 20/191) and sepsis (6.2%, 12/191). For 11 cases, the precise causes could not be identified (Table 8). It may be noted that the number of investigation cases were higher than MITS, as it includes data from the previous MITS also.
CHAMPS BANGLADESH Data: https://champs.iedcr.gov.bd/data